Borderline Personality Disorder: Understanding the Complexities

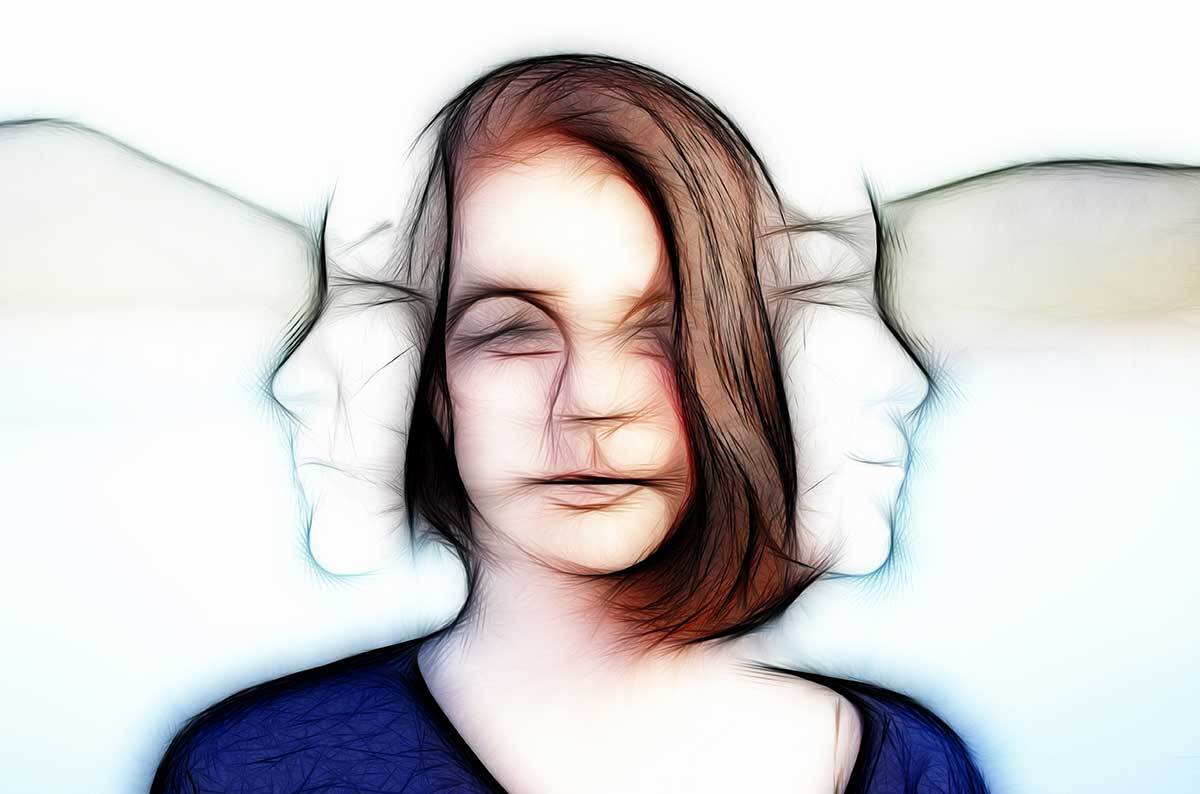
Borderline Personality Disorder (BPD) is a complex mental health condition characterised by a range of challenging symptoms. At its core is a profound fear of abandonment, which can lead to unstable relationships, impulsive behaviours, and intense emotional experiences. Individuals with BPD may struggle with a fluctuating sense of self, often experiencing rapid and extreme mood swings. These mood changes can manifest as inappropriate, intense anger, as well as chronic feelings of emptiness. Suicidal or self-harming behaviour is also common among those with BPD, highlighting the severity of the condition. Additionally, BPD can be accompanied by paranoid ideation, delusions, or severe dissociation, further complicating the individual's experience and perception of reality.
The instability and unpredictability of BPD can be challenging for both the individual and their loved ones to navigate. BPD is treatable, and with the right support and interventions, individuals can learn to manage their symptoms and improve their overall quality of life. Seeking professional help from mental health practitioners who specialise in BPD is crucial in addressing the complexities of this disorder.
Treatment options for BPD typically include psychotherapy, with Dialectical Behaviour Therapy (DBT) being particularly effective. DBT teaches individuals skills to manage intense emotions, improve interpersonal relationships, and develop mindfulness practices. Cognitive Behavioural Therapy (CBT) and Mentalization-Based Therapy (MBT) are also commonly utilised approaches.
In addition to therapy, medication may be prescribed to address specific symptoms such as depression, anxiety, or mood instability. However, no single medication is approved specifically for BPD, and pharmaceutical interventions are typically used in conjunction with psychotherapy.
Support groups and family therapy can also play a vital role in the treatment process, providing individuals with BPD and their loved ones with a space to share experiences, learn coping strategies, and build a supportive network. Developing a comprehensive treatment plan that addresses the unique needs of each individual is essential for achieving long-term stability and improving overall functioning.
Treatment for BPD typically involves a combination of psychotherapy and, in some cases, medication. Dialectical Behaviour Therapy (DBT) is widely recognised as one of the most effective therapeutic approaches for BPD. This form of cognitive-behavioural therapy focuses on teaching skills in mindfulness, emotion regulation, distress tolerance, and interpersonal effectiveness. Other evidence-based treatments include Mentalisation-Based Therapy (MBT) and Schema-Focused Therapy (SFT). These approaches aim to help individuals better understand their thoughts and emotions, develop healthier coping mechanisms, and improve their relationships with others.
While medication is not specifically approved for BPD, it may be prescribed to address co-occurring conditions such as depression, anxiety, or mood instability. However, medication should always be used in conjunction with psychotherapy for optimal results. The use of psychotropic medications in treating BPD symptoms requires careful consideration and close monitoring by a qualified mental health professional. Common pharmacological interventions may include selective serotonin reuptake inhibitors (SSRIs), mood stabilisers, or antipsychotics, depending on the individual's specific symptom profile and comorbidities.
It is crucial to emphasise that medication management alone is insufficient for comprehensive BPD treatment. A multifaceted approach, incorporating evidence-based psychotherapeutic modalities such as Dialectical Behaviour Therapy (DBT) or Mentalization-Based Treatment (MBT), is generally recommended. These therapeutic interventions aim to address the core features of BPD, including emotional dysregulation, interpersonal difficulties, and identity disturbance.
Furthermore, regular assessment of medication efficacy and potential side effects is paramount to ensure patient safety and treatment adherence. Clinicians should engage in ongoing dialogue with patients to adjust treatment plans as necessary and to promote a collaborative approach to care.
Recovery from BPD is a gradual process that requires commitment and patience. With consistent treatment and support, many individuals with BPD experience significant improvements in their symptoms and overall functioning. It is crucial for those affected by BPD to maintain a strong support network, including family, friends and mental health professionals, throughout their recovery journey.
The path to recovery often involves a combination of therapeutic approaches tailored to the individual's specific needs. Dialectical Behaviour Therapy (DBT), for instance, has shown remarkable efficacy in helping individuals manage intense emotions and improve interpersonal relationships. Alongside therapy, medication may be prescribed to address co-occurring conditions such as depression or anxiety.
It is important to note that recovery is not a linear process, and setbacks may occur. However, these should be viewed as opportunities for growth and learning rather than failures. As individuals progress in their recovery, they often develop improved coping mechanisms, enhanced emotional regulation skills, and a more stable sense of self.
Self-care plays a pivotal role in the recovery process. This may include maintaining a healthy lifestyle through proper nutrition, regular exercise, and adequate sleep. Engaging in mindfulness practices and stress-reduction techniques can also contribute significantly to emotional stability and overall well-being.